Developmental coordination disorder (DCD) is a condition that lasts a lifetime, and can make children appear to be clumsy. Children with DCD have trouble learning motor skills and coordinating the way they move. They might have trouble tying their shoes and buttoning buttons. In school, they may have trouble with writing, drawing, and sports. DCD is also known as dyspraxia and sensory-based motor disorder (SBMD).
Children with DCD may be late with developmental milestones such as crawling, walking, feeding themselves, and getting dressed without help. At first, a parent or a pediatrician may not see these delays as a sign of a condition. DCD may not be diagnosed until a child is five years old, or older.
While DCD affects both boys and girls, it is 3-4 times more common in boys. The condition seems to run in families. Experts think that at least 5 percent of children have DCD. The main treatment for DCD is occupational therapy (OT). If you think your child may have DCD, you should speak to your child’s doctor.
A child with DCD will not outgrow the condition, since it is a lifelong condition. Once diagnosed, however, a child with DCD can learn how to cope with the condition. Children can also do a great deal to improve their motor skills.
Is DCD a Learning Disability?
DCD isn’t thought of as a specific learning disability like dyslexia or dyscalculia. Experts think of it as a neurodevelopmental disorder, like ADHD. DCD often comes with or is comorbid with other issues or disabilities. Since the symptoms of various conditions can look the same or overlap, DCD may be confused with something else or misdiagnosed.
A child with DCD will not outgrow the condition, since it is a lifelong condition. Once diagnosed, however, a child can learn how to cope with the condition. A great deal can also be done to improve motor skills.
DCD Signs and Symptoms
DCD makes life a struggle both inside and outside of the classroom. In school, children with the condition may have trouble organizing their books, notebooks, pens, pencils, and erasers. They can have trouble taking notes or copying from the blackboard.
Outside the classroom, children may have trouble tying their shoes, pouring a bowl or cereal, or brushing their teeth. As DCD affects their balance, they may find it hard to sit on chair without constantly squirming. This can make eating difficult and messy.
DCD means that the skills that we call on to help us move, don’t work right. These movement skills include:
- Fine motor skills
- Gross motor skills
- Motor planning
- Coordinating movement (coordination)
When motor skills don’t work as they should, there may be problems with everyday life. Your child may find it hard to:
- Keep his/her balance
- Quickly change the way he or she is moving to avoid bumping into things or getting hurt
- Get his/her body to move the right way
- Learn new ways to move
- Predict what will happen when s/he moves this way or that
- Figure out and solve motor tasks (like buttoning a button)
Just Clumsy?
Most of us learn from experience. A child with DCD may not learn the right way to move from past mistakes. All of us have clumsy moments. We may misjudge how close a hand is to a glass a milk and knock it over. But after we clean up the mess and pour a fresh glass of milk, there are no more accidents. A child with DCD, on the other hand, may knock that glass of milk over again and again.
Children with DCD have trouble figuring out the order of how they must move to do a task. This is called sequencing. Trouble with sequencing can make it difficult to put one foot in front of the other when walking, for instance. That means that children with DCD may bump into other people, fall a lot, or drop things they are holding as they walk.
Kids don’t all learn to crawl, walk, and get dressed at exactly the same time. Some do these things earlier, and some later. That makes it hard to spot a problem like DCD. A parent or a pediatrician may think these delays are just normal for the child. They may think a child will outgrow being clumsy.
Once a child is in preschool, and the issues persist, it may become easier to see there is a real problem. That means that it is usually not until preschool that a child with DCD is diagnosed and given treatment. At that point, parents can look back and realize they were seeing the signs and symptoms of a real condition in their child, all along.
Signs and Symptoms by Age
Here are some signs of DCD in children, according to age:
Preschoolers
- Finds it hard to hold and use spoons and forks
- Finds it hard to throw a ball
- Doesn’t realize he or she is playing too roughly
- Is always bumping into other kids
- Squirms in his/her seat
- Can’t seem to sit upright
- Falls off of chairs
Kindergarten through Second Grade:
- Finds it hard to hold and use crayons, pencils, and scissors
- Can’t write letters the right way
- Can’t seem to get the spacing right between letters
- Going up and down the stairs is difficult
- Always bumping into people
- Still finds it hard to get dressed or brush his/her teeth
Third through Seventh Grade:
- Needs more time to write than the other kids
- It’s hard to cut up his/her food
- Still finds it hard to tie shoes or button buttons, so getting dressed is hard
- Math is difficult because s/he finds it difficult to line up the columns of numbers the right way
Eighth through Twelfth Grade:
- Finds it hard to type and text
- Has trouble with visual spatial tasks, for instance understanding how to work with shapes in geometry class.
- Finds it a daily challenge to open the latch on his/her school locker
- It’s hard to learn how to drive
DCD or something else?
It’s usual for children with DCD to also have learning disabilities or attention difficulties. The most common problem seen together with DCD is ADHD. Experts think that half of all children with DCD have ADHD, too.
Sometimes DCD seems to be something different. Kids with the condition have trouble sitting still or sitting up straight. They may squirm in their seats in an effort to keep their balance. Even a teacher with lots of experience may see the squirming and decide the child has ADHD. Or the child may have both DCD and ADHD, but the squirming and clumsiness can make the experts miss the DCD part of the problem.
To confuse things further, other issues can make children fidget or squirm. Sensory processing issues can cause these behaviors. A label inside a shirt collar can drive a kid with sensory processing problems to squirm and fidget every bit as much as a child with DCD, trying to sit still in his/her chair.
But DCD can just look like other issues. For example, because of balance problems, these kids often have trouble sitting upright or sitting still. They may move around a lot to keep their bodies up.
Conditions with similar symptoms
There are many issues that can come with DCD or be confused with the condition, including:
- ADHD
- Autism
- Dysgraphia
- Executive functioning issues
- Mental health issues such as anxiety
- Processing speed issues
- Sensory processing issues
Because DCD may be confused with or come along with other conditions, it’s important for a child to have a full evaluation. That way, if a child has other issues, these too will be diagnosed and treated.
DCD Risk Factors
We don’t know what causes DCD. We do know some of the risk factors, including:
- Male gender
- Small for size at birth
- Born early, before the 37th week
- Low birth weight
- Family history of DCD
- Maternal alcohol or drug use during pregnancy
Evaluating your child
If you suspect your child may have DCD, see your child’s doctor. Your child’s pediatrician may be able to diagnose the condition. Or the pediatrician may work with other experts, for instance, a developmental behavioral pediatrician, a pediatric neurologist or a child psychologist, to evaluate and diagnose the problem.
The most common ages to evaluate for DCD are 5 and 6. Evaluators will look at motor and cognitive skills. They’ll ask questions about other factors that could be having an impact, too, in school and home life. They’ll also want to know whether your child has hit certain milestones in development and when symptoms began.
Evaluating children for DCD calls for assessing how your child moves. Here are some of the movement skills that evaluators will seek to assess:
- Balance
- Coordination
- Fine motor control
- Motor planning
- Range of motion
- Strength
The evaluators will want to see how well your child moves by having him do things like cut out paper shapes with a scissors, or string beads. Your child may be asked to draw different shapes or color a picture, to see how well s/he stays within the lines. These tasks show a child’s visual perception skills.
Therapy for DCD
The main treatment for DCD is occupational therapy (OT). An occupational therapist will work with your child to improve movement and motor skills. In order to improve handwriting skills, for instance, the occupational therapist may have your child practice tracing letters. A child who struggles with tying shoelaces, can practice on a lacing board.
Children with DCD who have an IEP or a 504 plan, may be able to receive OT for free in school. You may be able to get OT covered through your insurance plan. You can also hire a private occupational therapist.
Some children with DCD also need to work with a physical therapist. Physical therapy can help improve balance and strengthen muscle tone.
In school, children with DCD may need accommodations to manage their schoolwork. They may need extra time for tests or written work, because writing is difficult. Assistive technology for instance speech-to-text tools that can take dictation, can also be a big help in getting a child with DCD through school. The teacher may be willing to let your child use these accommodations in the classroom. Otherwise, your child can receive formal accommodations with an IEP or 504 plan.
Love and Support
The most important thing you can do for your child with DCD is to offer support and understanding for the challenges your child will confront every day. Advocating for your child is part of that. You may have to explain that your child didn’t mean to bump into his friend yet again, or that your child has trouble sitting still, because he has DCD. When you mention DCD, you can expect to be met with blank stares—sometimes even from your child’s teachers. (You can always tell people that Harry Potter actor Daniel Radcliffe also has DCD—to Google it!)

Help your child break down difficult tasks into smaller parts and offer lots of practice on a regular basis. Find ways to change tasks so they become easier. You might, for instance, use special grips for pencils and pens that make them easier to hold. With occupational therapy, physical therapy, help at home, and accommodations in and out of the classroom, your child is bound to improve his or her motor skills to some degree.
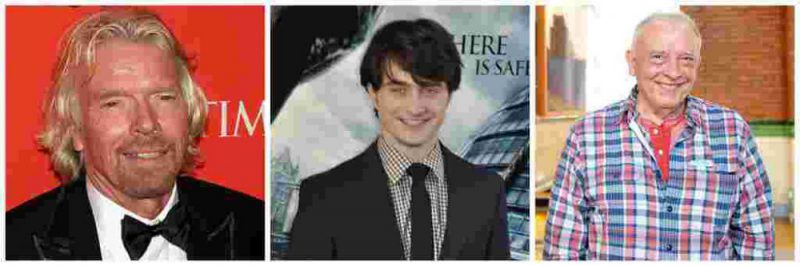
Be patient and always remember that it’s not easy to live with DCD. Encourage your child however you can and always be ready with your sympathy and understanding. Remind your child that many great and successful people have DCD. (In addition to actor Daniel Radcliffe, there’s entrepreneur Richard Branson and photographer David Bailey—imagine having to hold that camera still!) Most of all, let your child know your love is there to be counted on, no matter what happens today or any other day, in or out of the classroom.




Thanks a lot Varda Epstein from my heart for your priceless informative post. My little angel (daughter) are sufferer with this Developmental coordination disorder about 2 years. Hopefully, this post help me a lot because i have no more information on it.